Twenty years ago, the fight against cancer seemed as if it were about to take a dramatic turn.
Traditionally, cancer doctors fought the disease with crude weapons, often simply poisoning fast-growing cells whether they were cancerous or healthy. But then a team of researchers hit on a new strategy: drugs targeting proteins produced by cancer cells that seemed necessary to their survival.
Once such drug, Gleevec, worked spectacularly in patients with chronic myeloid leukemia. But the clinical trials that followed mostly have produced disappointments. According to a study published earlier this year, only 3 percent of cancer drugs tested in clinical trials between 2000 and 2015 have been approved to treat patients.
A study published on Wednesday in the journal Science Translational Medicine offers one reason for the failure: Scientists are going after the wrong targets.
“I hope people will really wake up to the need to be much more rigorous,” said Dr. William Kaelin, a professor of medicine at Harvard University who was not involved in the new study.
Jason Sheltzer, a cancer biologist at Cold Spring Harbor Laboratory in New York State, and his colleagues made the discovery as they were trying to come up with a new test for breast cancer.
In certain forms of the disease, cancer cells make high levels of a protein called MELK. Extremely high levels can mean poor odds of survival for the patient.
Earlier studies had indicated that MELK was essential to the spread of the cancer; indeed, researchers were already testing a drug for breast cancer that targets the MELK protein.
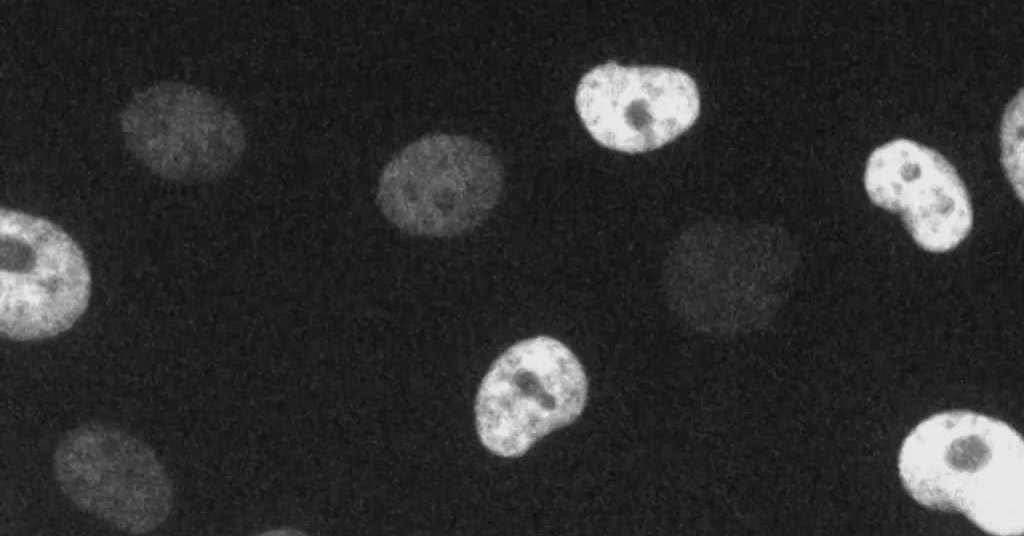
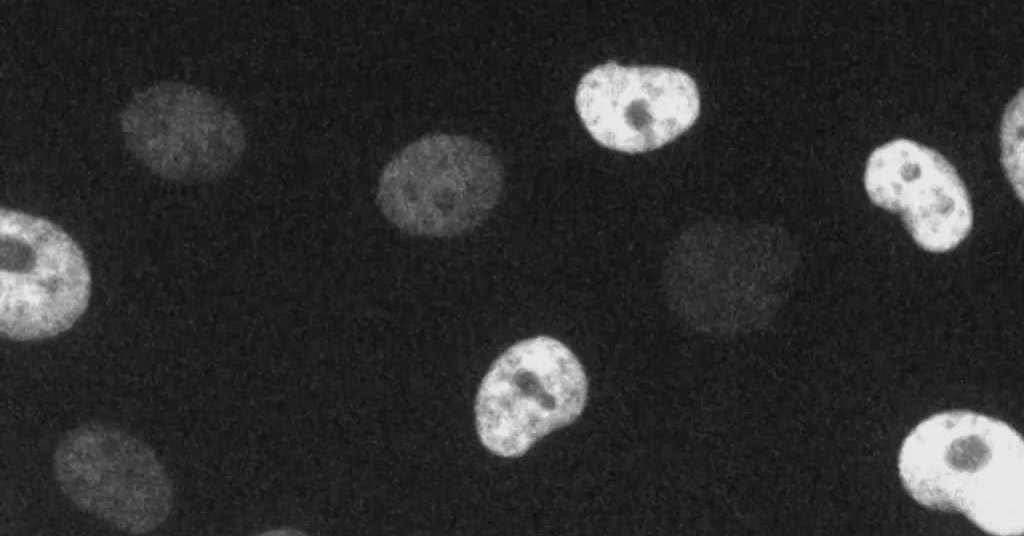
Two undergraduates in Dr. Sheltzer’s lab, Ann Lin and Christopher J. Giuliano, used Crispr, the revolutionary DNA-editing tool, to snip out the gene for MELK in cancer cells. The cells should have stopped growing, but to the surprise of the scientists, they did not.
“The cancer cells did not care whatsoever,” Dr. Sheltzer said.
It was odd that the cells didn’t need a supposedly essential gene. Odder still was what happened when the scientists exposed the cells to the MELK-targeting drug. It stopped the cancer cells anyway — even though they lacked the gene that the drug targeted.
Dr. Seltzer wondered if he simply had stumbled across a peculiar case. So he widened his research, running the same experiment with 10 other drugs. All were protein-targeting medications currently in clinical trials.
With each drug, the scientists got the same results. Every supposedly essential protein turned out to be expendable in the cancer cells, yet all these cells stopped growing when the scientists applied the drug.
This sort of mistake may lead to failures in clinical trials, Dr. Sheltzer said. “When you design a clinical trial, you want to pick out the patients who are most likely to respond,” he said. “That trial may fail because you’re picking the wrong people to give that drug to.”
The mistakes Dr. Sheltzer has uncovered may have come about because the scientists who were hunting for drug targets used unreliable tools.
“A lot of the drug targets that are in clinical trials today were discovered with the best technology from five or 10 years ago,” he said.
That technology, known as RNAi, seemed at the time like it could zero in on cancer targets with high precision. “Everyone thought finally we had the genie in the lamp,” Dr. Kaelin said.
[Like the Science Times page on Facebook. | Sign up for the Science Times newsletter.]
RNAi allows scientists to craft a molecule to block cells from making a particular protein. If blocking a protein’s production stopped cancer cells from growing, scientists looked for a drug that also targeted that protein.
But some critics questioned whether RNAi was all that precise. The technique may block not just a target protein, but certain others as well. Dr. Sheltzer tested this possibility with one of the drugs in his experiment, OTS964.
The researchers gave the drug to colonies of cancer cells with the target protein removed. Most still died — but a few did not.
The researchers sequenced the DNA of the surviving cells. It turned out they all had mutations in the same gene, which encodes a protein called CDK11B.
No one had any idea that the protein was essential to the survival of the cancer cells. But Dr. Sheltzer’s experiment suggested it was: The mutant cells survived because they had an altered form of the protein, with which the drug could not interfere.
When the researchers cut out the CDK11B gene, the cancer cells died — further evidence that the protein was necessary to the cancer cell.
Traver Hart, a cancer biologist at M.D. Anderson Cancer Center in Houston who was not involved in the new study, said that scientists need to take another look at cancer drugs now undergoing testing.
“There clearly exists a legacy of RNAi-guided bad targets that needs to be purged from the drug development pipeline,” he said.
That doesn’t mean that targeting essential proteins is pointless. Scientists just need to make sure they’re going after the right ones.
Searching for mutations in the genes of cancer cells may be one way to avoid false positives. Instead of relying on hunches about what is a good target, cancer cells might speak for themselves.
“There is probably a whole universe of unexplored drug targets in the cancer cell,” Dr. Sheltzer said.