In recent years, health officials have pushed aggressively to include more women in clinical trials of new drugs. Gone is the ban that once excluded women of childbearing age from participating in studies. Even scientists who work with animals are now encouraged to include mice and rats of both sexes.
But when it comes to breast cancer, it is men who get short shrift. They are often excluded from clinical trials of new treatments. When new breast cancer drugs come to market, there is little data to indicate whether they are safe or effective in men. Some new drugs are approved only for women.
The disease is extremely rare in men, who account for fewer than 1 percent of breast cancer cases. Nonetheless, the Food and Drug Administration is calling on researchers to include male patients in clinical trials of breast cancer treatments, even if the studies are unlikely to enroll more than a handful of male patients.
The guidance is a draft recommendation now open to public comment. Some breast cancer specialists called it a long overdue step.
“It’s so frustrating in clinic to see patients and say, ‘Well, we don’t really know — the drugs have been tested in women. We think it should work in men, but there’s no real evidence to back that up,’” said Dr. Sharon Giordano, a professor of breast medical oncology at M.D. Anderson Cancer Center in Houston who treats many male patients.
Even if only a few men participate in each trial, data on them could be pooled. Coupled with real-world experience using the medications, that data could shed light on treatment of men, she said.
The proposed guideline comes amid growing concerns that men with breast cancer — whose disease tends to be diagnosed in more advanced stages — are often not getting optimal care and may be missing out on lifesaving therapies.
One of the largest analyses of these patients, published in Annals of Oncology in 2017, reported what the authors called “troublesome findings.” The study, carried out by the International Male Breast Cancer Program, analyzed 1,500 men with breast cancer in Canada, the United States and seven European countries.
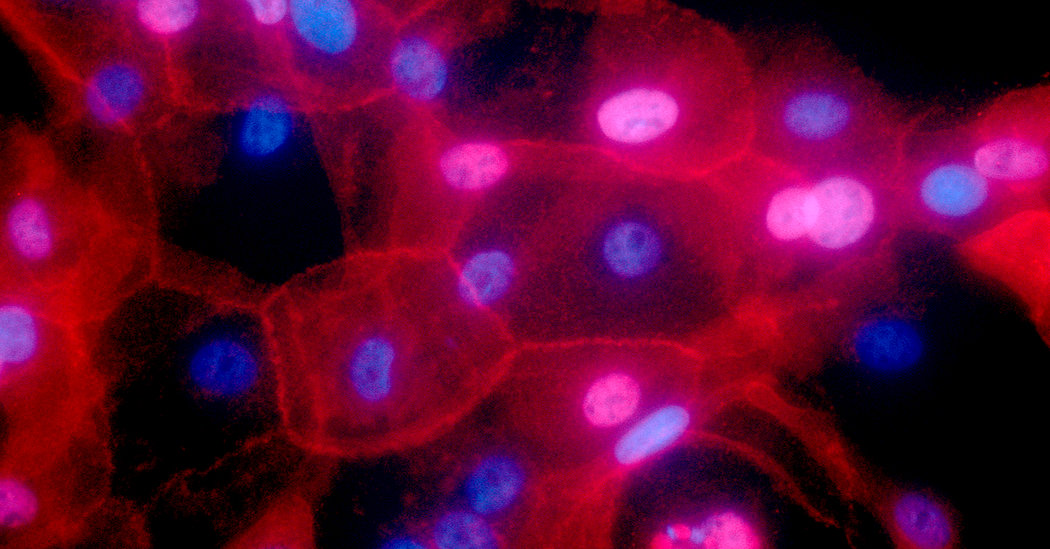
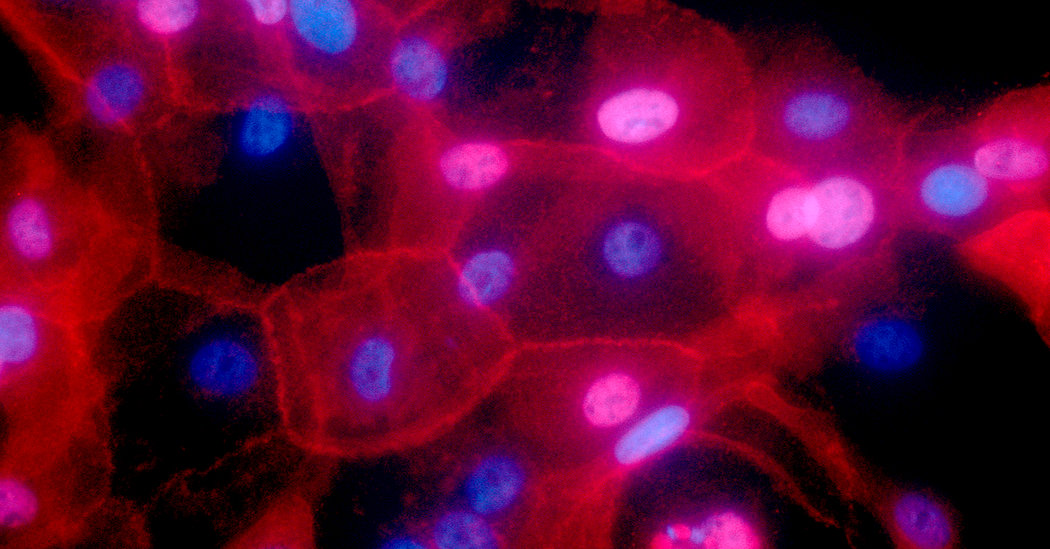
The vast majority of men with breast cancer have tumors that are fueled by estrogen. (Men produce the hormone, too.) In the study, virtually all men whose cancer had not spread had estrogen-receptor-positive tumors, which should be treated with therapy to reduce estrogen levels in the body or to block the hormone from attaching to breast cancer cells.
But only 77 percent of these patients received anti-estrogen therapy, the study found. That means that nearly one in five men who should have received a potentially lifesaving therapy did not get it, said Dr. Fatima Cardoso, the lead author of the study and director of the breast unit at Champalimaud Clinical Center in Lisbon. “We don’t know why,” she said.
The most common treatment for men was surgery: a mastectomy to remove the breast, or a lumpectomy to remove the tumor. But the men had low rates of radiation treatment, which is standard care after a lumpectomy and often recommended after a mastectomy if, for example, the tumor is very large, said Dr. Marisa C. Weiss, founder of Breastcancer.org. The study called the low rates a “major concern.”
Poor care is all too common when patients suffer from rare diseases, and for men, breast cancer is a rare disease, Dr. Cardoso noted.
“Many, many oncologists have never seen a case of breast cancer in a male patient,” she said. For these patients, she added, it’s particularly important to find experienced doctors.
Men with breast cancer are often older. They may have very large tumors by the time they seek care, because they were not on the lookout for the disease.
[Like the Science Times page on Facebook. | Sign up for the Science Times newsletter.]
“Some men are not even aware they have breasts and not aware they can have breast cancer,” Dr. Cardoso said. “Even health professionals often don’t think about it. General practitioners who see male patients don’t pay attention to the breast.”
“We need a lot of education to remind men they have breasts, too, and should check them,” she said. “And if they find something, go to the oncologist fast.”
Dr. Cardoso and other experts welcomed the proposed new guidelines, but said researchers should collaborate on large international trials focused on men with breast cancer. When the patient population is small, large trials are needed to make significant findings.
“Some data is better than no data, but it’s not the ultimate solution,” said Dr. Larry Norton, chairman of clinical oncology at Memorial Sloan Kettering Cancer Center in New York.
But pharmaceutical companies are not very interested in funding such trials. “No one wants to invest in a disease that is only 1 percent of all breast cancers,” Dr. Cardoso said.
As with women, one of the first warning signs of breast cancer in men can be a lump in the breast. Other possible early symptoms include nipple pain, discharge from the nipple, a sore on the nipple or areola, an inverted nipple, or swollen lymph glands under the arm.
The risk of breast cancer in men increases with age, and is higher in men who have high estrogen levels or genetic mutations, or who have been exposed to radiation. Men with Klinefelter syndrome — who carry an extra X chromosome — are also at increased risk.
Family history is important: Doctors recommend all men with breast cancer be tested for mutations in the BRCA1 or BRCA2 genes, which are linked to both breast and ovarian cancer in women.
Men who have mutations in these genes are 80 times as likely to develop breast cancer as men without these mutations. A positive result alerts female relatives that they may need to be tested, as well.