In early 2021, scientists in Colombia discovered a worrisome new coronavirus variant. This variant, eventually known as Mu, had several troubling mutations that experts believed could help it evade the immune system’s defenses.
Over the following months, Mu spread swiftly in Colombia, fueling a new surge of Covid-19 cases. By the end of August, it had been detected in dozens of countries, and the World Health Organization had designated it a “variant of interest.”
“Mu was starting to make some noise globally,” said Joseph Fauver, a genomic epidemiologist at the University of Nebraska Medical Center and an author of a recent study on the variant.
And then it fizzled. Today, the variant has all but vanished.
For every Delta or Omicron there is a Gamma, Iota or Mu, variants that drove local surges but never swept to global dominance. And while understanding Omicron remains a critical public health priority, there are lessons to be learned from these lesser lineages, experts say.
“This virus has no incentive to stop adapting and evolving,” said Joel Wertheim, a molecular epidemiologist at the University of California San Diego. “And seeing how it did that in the past will help us prepare for what it might do in the future.”
Studies of the also-rans have shed light on surveillance gaps and policy blunders — providing more evidence that America’s international travel bans were not effective — and on what makes the virus successful, suggesting that in the early phase of the pandemic, transmissibility was more important than immune evasion.
The research also highlights how much context matters; variants that make an impact in some places never gain a foothold in others. As a result, predicting which variants will surge to dominance is difficult, and staying on top of future variants and pathogens will require comprehensive, nearly real-time surveillance.
“We can gain a lot by looking at the viral genomic sequence and saying, ‘This one is probably worse than another one,’” Dr. Wertheim said. “But the only way to really know is to watch it spread, because there are a whole lot of potentially dangerous variants that never took hold.”
Here’s looking at Mu
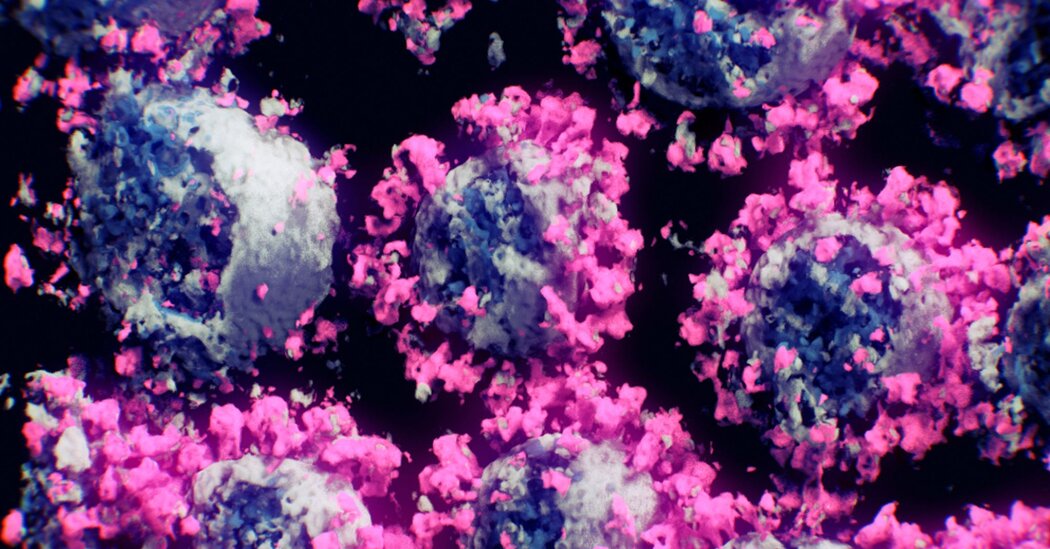
The coronavirus is constantly changing, and most new variants never get noticed or named. But others raise alarms, either because they quickly become more common or because their genomes look ominous.
Both were true of Mu as it spread in Colombia. “It contained a couple of mutations that people had been watching very closely,” said Mary Petrone, a genomic epidemiologist at the University of Sydney and an author of the new Mu paper. Several of the mutations in its spike protein had been documented in other immune-evasive variants, including Beta and Gamma.
In the new study, which has not yet been published in a scientific journal, scientists compared Mu’s biological characteristics to those of Alpha, Beta, Delta, Gamma and the original virus. Mu did not replicate faster than any other variant, they found, but it was the most immune-evasive of the bunch — more resistant to antibodies than any known variant besides Omicron, Dr. Fauver said.
By analyzing the genomic sequences of Mu samples collected from all over the world, the researchers reconstructed the variant’s spread. They concluded that Mu had likely emerged in South America in mid-2020. It then circulated for months before it was detected.
Genomic surveillance in many parts of South America was “patchy and incomplete,” said Jesse Bloom, an expert in viral evolution at the Fred Hutchinson Cancer Research Center in Seattle. “If there had been better surveillance in those regions, possibly it would have been easier to make a faster assessment of how worried to be about Mu.”
Mu presented another challenge, too. It happened to have a type of mutation, known as a frameshift mutation, that was rare in coronavirus samples. Such mutations were flagged as errors when scientists, including Dr. Fauver, tried to upload their Mu sequences to GISAID, an international repository of viral genomes used to keep tabs on new variants.
That complication created delays in the public sharing of Mu sequences. The time that elapsed between when a virus sample was collected from a patient and when it was made publicly available on GISAID was consistently longer for Mu cases than for Delta cases, the researchers found.
“The genome itself was basically creating artificial surveillance gaps,” Dr. Fauver said. “It resulted, at least in our experience, in us not getting data out for weeks when normally we’re trying to get it out in days.”
(GISAID’s quality-control systems are important, the researchers stressed, and the repository has fixed the issue.)
Combine these surveillance gaps with Mu’s immune evasiveness and the variant seemed poised to take off. But that is not what happened. Instead, Mu radiated from South and Central America to other continents but did not circulate widely once it got there, the scientists found. “That was an indication that this variant was not as fit necessarily in maybe the North American and European populations as we had expected,” Dr. Petrone said.
That was likely because Mu found itself competing with an even more formidable variant: Delta. Delta was not as skilled at dodging antibodies as Mu, but it was more transmissible. “So, in the end, Delta spread more widely,” Dr. Bloom said.
Right variant, right time
Studying successful variants tells only half the story. “Variants that do not become dominant are, in a way, negative controls,” Dr. Petrone said. “They tell us what didn’t work, and, in doing so, help to fill in knowledge gaps around variant fitness.”
Delta overtook several immune-evasive variants besides Mu, including Beta, Gamma and Lambda. This pattern suggests that immune evasion alone was not enough to allow a variant to outdo a highly transmissible version of the virus — or at least it wasn’t during the early phase of the pandemic, when few people had immunity.
But vaccinations and multiple waves of infection have changed the immune landscape. A highly immune-evasive variant should now have more of an edge, scientists said, which is likely part of the reason Omicron has been so successful.
Another recent study suggested that in New York City immune-evasive Gamma tended to do better in neighborhoods with higher levels of pre-existing immunity, in some cases because they were hit hard in the first Covid wave. “We can’t view a new variant in a vacuum, because it comes about in the shadow of all of the variants that came before it,” said Dr. Wertheim, who was an author of the study.
Indeed, the clash of variants past reveals that success is highly dependent on context. For example, New York City may have been the birthplace of the Iota variant, which was first detected in virus samples collected in November 2020. “And so it got a foothold early on,” said Dr. Petrone. Even after the more transmissible Alpha variant arrived, Iota remained the city’s dominant variant for months, before eventually fading away.
But in Connecticut, where Iota and Alpha both appeared in January 2021, things unfolded differently. “Alpha just kind of took off immediately, and Iota didn’t stand a chance,” said Dr. Petrone, who led a study of the variants in the two regions.
A similar pattern is already beginning to play out with Omicron’s multiple lineages. In the United States, BA.2.12.1, a subvariant first identified in New York, has taken off, while in South Africa, BA.4 and BA.5 are driving a new surge.
That’s another reason to study variants that waned, said Sarah Otto, an evolutionary biologist at the University of British Columbia. A variant that was poorly matched for a certain time and place could take off in another. Indeed, Mu’s misfortune might have simply been that it emerged too soon. “There might not have been enough people that had immunity to really give that variant a boost,” Dr. Otto said.
But the next variant of concern could be a descendant of, or something similar to, an immune-evasive lineage that never quite took hold, she said.
Looking back at previous variants can also provide insight into what worked — or didn’t — in containing them. The new Gamma study, provides further evidence that international travel bans, at least as the United States implemented them, are unlikely to prevent a variant’s global spread.
Gamma was first identified in Brazil in late 2020. In May of that year, the United States barred most non-U.S. citizens from traveling into the country from Brazil, a restriction that remained in place until November 2021. Yet Gamma was detected in the United States in January 2021 and soon spread to dozens of states.
Because Gamma never came to dominate worldwide, studying its spread provided a “cleaner” picture of the effectiveness of travel bans, said Tetyana Vasylyeva, a molecular epidemiologist at the University of California San Diego and an author of the study. “When it comes to studying variants like, let’s say, Delta — something that has caused a major outbreak in every place — it is really difficult at times to find patterns, because it happens on a very large scale and very fast,” she said.
In an ongoing global health emergency, with a virus that changes fast, there is an understandable impulse to focus on the future, Dr. Fauver said. And as the world’s attention turned to Delta and then Omicron, he and his colleagues discussed whether to continue their study of old-news Mu.
“We were like, ‘Does anyone care about Mu anymore?’” Dr. Fauver recalled. “But we think there’s still room for high-quality studies that ask questions about previous variants of concern and try to look back on what happened.”
