“These results suggest bundled payments are a win-win,” said Ezekiel Emanuel, a co-author of the study. “They save payers like Medicare money and encourage hospitals and physicians to be more efficient in the delivery of care.”
But Robert Berenson, a fellow at the Urban Institute, urges some caution. “Studying one kind of procedure doesn’t tell you much about the rest of health care,” he said. “A lot of health care is not like knee and hip replacements.”
Michael Chernew, a Harvard health economist, agreed. “Bundles can certainly be a helpful tool in fostering greater efficiency in our health care system,” he said. “But the findings for hip and knee replacements may not generalize to other types of care.”
Christine Yee, a health economist with the Partnered Evidence-Based Policy Resource Center at the Boston Veterans Affairs Healthcare System, has studied Medicare’s previous efforts and summarized studies about them. (I and several others were also involved in compiling that summary.) “Medicare has tried bundled payments in one form or another for more than three decades,” Ms. Yee said. “They tend to save money, and when post-acute care is included in the bundle, use of those kinds of services often goes down.”
One limitation shared by all of these studies is that they are voluntary: No hospital is required to participate. Nor are they randomized into the new payment system (treatment) or business as usual (control). Therefore we can’t be certain that apparent savings are real. Maybe hospitals that joined the bundled payment programs are more efficient (or can more easily become so) than the ones that didn’t.
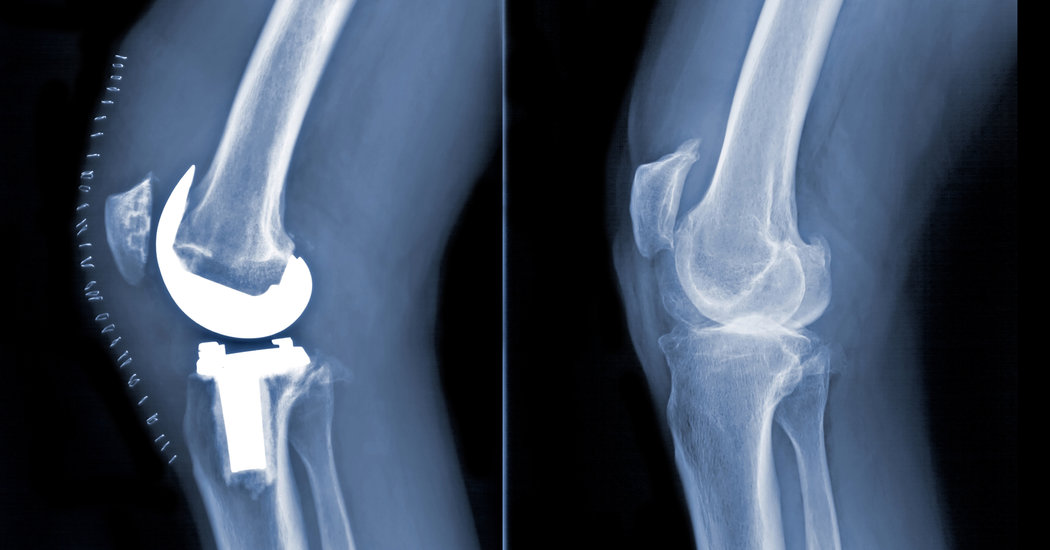
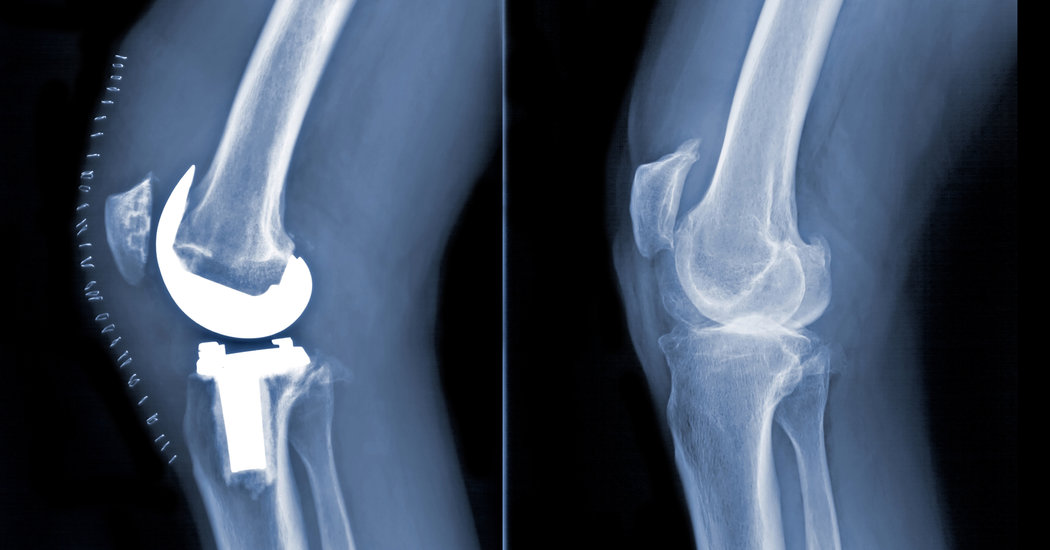
Another new study in JAMA examines a mandatory, randomized trial of bundled payments. On April 1, 2016, Medicare randomly assigned 75 markets to be subject to bundled payments for knee and hip replacements and 121 markets to business as usual. This policy experiment, known as the Comprehensive Care for Joint Replacement program, will continue for five years. The JAMA study analyzed just the first year of data.
“In this first look at the data, we examined post-acute care because it is an area where there is concern about overuse,” said Amy Finkelstein, an M.I.T. health economist and an author of the study. “In addition, prior work suggested that it’s a type of care that hospitals can often avoid.”