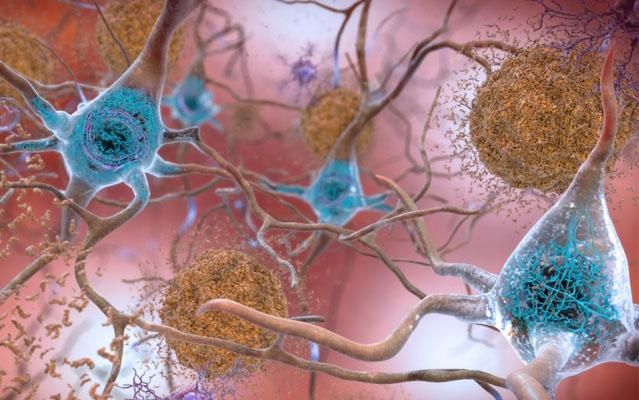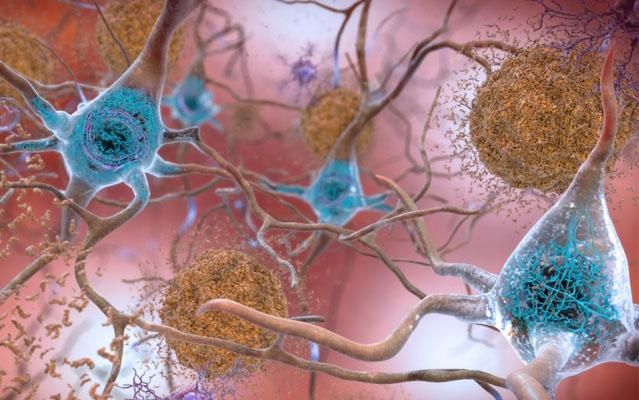
IMAGE: In brains affected by Alzheimer’s disease, abnormal levels of the beta-amyloid protein clump together to form plaques (seen in brown) that collect between neurons and disrupt cell function. Abnormal collections… view more
Credit: National Institute on Aging, NIH
Among the confounding challenges of diagnosing and treating Alzheimer’s disease (AD) is the fact that patients with asymptomatic and symptomatic versions of the degenerative condition may share similar neuropathological burdens but experience significantly different rates of cognitive decline.
In a new study, published July 23, 2019 in Cell Reports, a team led by researchers at University of California San Diego School of Medicine used the transcriptome — the sum of all messenger RNA (mRNA) molecules expressed from genes — to compare 414 study participants with clinically diagnosed and neuropathologically confirmed AD with an age-matched, non-demented control group from a community-based neuropathological study.
Their findings suggest that integrating protein interactions with gene perturbations can generate a comprehensive framework for characterizing alterations in the molecular network related to AD.
While familial AD has a strong genetic factor, the causes of sporadic AD (the most common form) are multiple and not completely known. Primary risk factors include age, gender and family history, but also include a variety of biological, psychological and social factors.
Much research has focused upon two key elements of AD pathology — the accumulation of amyloid protein plaques and abnormal neurofibrillary tau protein tangles in the brain, which are thought to cause dysfunction and death of neurons. But scientists increasingly recognize the relevance and importance of other factors, such as inflammation, blood circulation problems and brain atrophy — all of which “correlate with clinical symptoms of cognitive decline and have led to changes in diagnostic criteria during the last decade,” wrote the authors.
The new study combined analyses of gene perturbations and protein interactions, said senior author Robert Rissman, PhD, professor of neurosciences at UC San Diego School of Medicine, director of the Biomarker Core for the Alzheimer’s Disease Cooperative Study (ADCS) and director of the Neuropathology/Brain Bank and Biomarker Cores for the UC San Diego Shiley-Marcos Alzheimer’s Disease Research Center, which ultimately identified functionally distinct composite clusters of genes revealing extensive changes in expression levels in AD. These clusters broadly corresponded to synaptic transmission, metabolism, cell cycle, cell survival and immune response — all critical aspects involved in AD pathology.
“One of the big problems in AD research is identifying patients at risk at the right time,” said Rissman. “Understanding the gene networks that may change in specific patient groups can help streamline clinical trials recruitment efforts and reduce costs and time to enroll trials. With the field shifting more and more toward pre-symptomatic disease, we need to expand our understanding of the molecular mechanisms that underlie the entire disease spectrum.”
###
Co-authors include: Saranya Canchi, UC San Diego and Veterans Affairs San Diego Healthcare System; Balaji Raao, Deborah Masliah, Sara Brin Rosenthal, Roman Sasik and Kathleen M. Fisch, all at UC San Diego; Philip L. De Jager, Columbia University Medical Center; and David A. Bennett, Rush University Medical Center.
Disclaimer: AAAS and EurekAlert! are not responsible for the accuracy of news releases posted to EurekAlert! by contributing institutions or for the use of any information through the EurekAlert system.