Pfizer announced on Tuesday that its Covid pill was found to stave off severe disease in a key clinical trial and that it is likely to work against the highly mutated Omicron variant of the virus. The results underscore the promise of the treatment, which health officials and doctors are counting on, to ease the burden on hospitals as the United States braces for a mounting fourth wave of the pandemic.
If the Food and Drug Administration authorizes the drug, which could happen within days, then patients might begin receiving it by the end of the year. Although supply will be limited at first, public health experts are hopeful that the pills might curb the worst outcomes from the disease, no matter the variant.
Pfizer said its antiviral pill was found to reduce the risk of hospitalization and death by 88 percent when given to unvaccinated people at high risk of severe Covid within five days of the onset of symptoms. The company also said that laboratory experiments indicated that the drug will attack a key protein in the Omicron variant, which is surging in South Africa and Europe and is expected to dominate U.S. cases in the weeks ahead.
“This is quite amazing and potentially transformative,” said Sara Cherry, a virologist at the Perelman School of Medicine at the University of Pennsylvania who was not involved in the study. “If we could keep people out of hospitals, that would have a huge impact on health care.”
Some U.S. states are seeing record high hospitalizations as the Delta variant continues to spread, mostly among the unvaccinated. And researchers are now warning that Omicron may spread even more rapidly and seems to evade some of the immune defenses provided by vaccines or previous infection.
In a study released on Tuesday, South African researchers found that two doses of the Pfizer-BioNTech vaccine provide much less protection against infection with Omicron than against other variants.
Although the shots still provide strong protection against severe disease and hospitalization, it’s possible that Omicron’s drastic rate of transmissibility will create a surge of severe infections, particularly in unvaccinated people. Those seriously ill people could swamp hospitals in the next few months. A highly effective antiviral pill like Pfizer’s could be crucial to easing that surge, Dr. Cherry said.
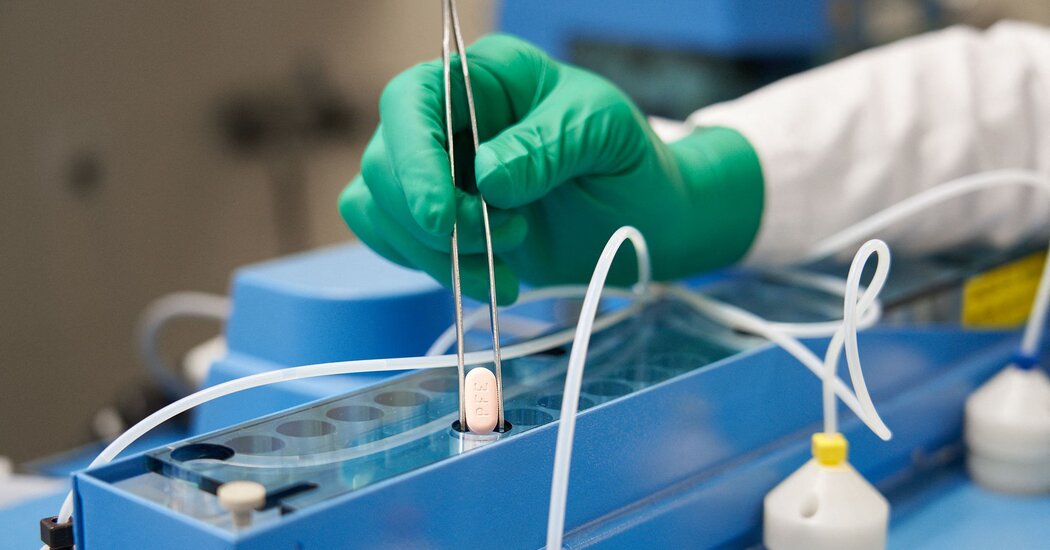
Last month, Pfizer asked the Food and Drug Administration to authorize the treatment, known as Paxlovid, for high-risk adults, based on a preliminary batch of data. The new results will undoubtedly strengthen the company’s application for the drug, which is meant to be prescribed by a health care provider after a positive virus test and taken at home.
The results, based on an analysis of more than 2,200 unvaccinated volunteers at high risk of severe disease, largely match the company’s initial, smaller analysis of the clinical trial, released last month.
Pfizer said that in its final analysis, 0.7 percent of patients who received Paxlovid were hospitalized within 28 days of entering the trial, and none died. By contrast, 6.5 percent of patients who received a placebo were hospitalized or had died.
Pfizer also released preliminary data from a separate trial looking at people with a lower risk. These volunteers included vaccinated people who carried a risk factor for severe disease, as well as unvaccinated patients with no risk factors.
Among this group of 662 volunteers, Paxlovid reduced the risk of hospitalization and death by 70 percent, the company said.
Several public health experts said they thought it was unlikely that the F.D.A. would immediately authorize Paxlovid for people at standard risk of becoming severely ill from Covid based on the preliminary results, though the agency may do so eventually.
“Maybe it’s something that your physician would think about if you had severe underlying conditions,” Seema Lakdawala, a virologist at the University of Pittsburgh, said.
Dr. Lakdawala said that regulators might consider expanding the drug’s use if the benefits outweighed any potential risks. Paxlovid might shorten the amount of time that people shed the coronavirus, for example, which could, in turn, reduce how long people have to spend in quarantine. It might even cut down the chances that infected people pass on the virus to others. “All of those would be hugely beneficial,” she said.
These possibilities would first have to be confirmed in trials, Dr. Lakdawala cautioned. Pfizer is running a trial to see how well Paxlovid can block transmission in households and expects results in the first half of 2022.
Mikael Dolsten, the chief scientific officer of Pfizer, was exuberant about the results after having overseen the development of the drug since the spring of 2020, with more than 200 company scientists crafting the molecule and then testing it in animals and people.
While the drug was in development, Dr. Dolsten held out hope that it might be 60 percent effective. Its true potency left him stunned. “We really hit the top of the board,” he said in an interview.
In both trials, most of the volunteers carried the Delta variant. But Pfizer said on Tuesday that in laboratory experiments, Paxlovid also performed well against the highly mutated Omicron variant. The drug jams into one of Omicron’s crucial proteins — called a protease — just as effectively as it does with other variants, Pfizer found.
Dr. Cherry said that the experiment Pfizer ran was a good first pass at testing the treatment against Omicron. But she and other scientists will be receiving Omicron viruses this week from labs where it’s now being grown, after which they can directly test Paxlovid to see how well it stops the viruses from invading cells. “We hope to start those experiments this week,” Dr. Cherry said.
Pfizer’s treatment is meant to be taken as 30 pills over five days. Patients will take three pills at a time: two of Pfizer’s new pills and one of the low-dose H.I.V. drug known as ritonavir, which helps Pfizer’s drug remain active in the body longer.
The Coronavirus Pandemic: Key Things to Know
Pfizer’s Covid pill. A study of Pfizer’s oral Covid treatment confirmed that it helps stave off severe disease, even from the Omicron variant, the company announced. Pfizer said the treatment reduced the risk of hospitalization and death by 89 percent if given within three days of the onset of symptoms.
Ritonavir can interfere with certain medications, including common ones for cholesterol and cardiovascular issues, potentially causing serious side effects. But doctors usually worry about those interactions only when H.I.V. patients take the drug for years. With Pfizer’s five-day treatment, doctors might recommend that patients simply stop taking certain drugs like statins for a few days. But with other drugs for which treatment cannot be easily interrupted, like blood thinners and immunosuppressive medications, patients may need to adjust their dosage or be monitored while on Pfizer’s treatment.
“The risk is going to vary a lot by what drug we’re talking about,” said Conan MacDougall, an infectious disease pharmacist at the University of California San Francisco.
Health officials have been waiting for a convenient option like Paxlovid since the start of the pandemic. They are counting on the pills to reach many more people than the cumbersome monoclonal antibody treatments, which are typically given at a hospital or clinic. Several brands of antibody treatments may not work as well against Omicron.
Still, there are logistical obstacles that could limit the Pfizer treatment’s promise, experts cautioned. To receive the pills, patients are expected to need a positive coronavirus test and a prescription from a health care provider, all within five days after developing symptoms. Those challenges could be especially pronounced among the people most vulnerable to becoming severely ill from Covid.
The federal government has ordered enough of Pfizer’s pills to cover 10 million people, at a cost of about $530 per patient. Pfizer will have about 180,000 treatment courses ready by the time it receives its expected authorization this month, but some of those will most likely go to countries other than the United States. The company is expected to deliver only enough of its pills to cover 300,000 Americans before the end of February, and then sharply increase the pace of its deliveries.
“There’s probably some tempered expectations that are needed, because this is not available today. It’s not going to be available a month from now for the average person. It’s going to be something that slowly gets rolled out,” said Dr. David Boulware, an infectious disease specialist at the University of Minnesota.
Pfizer’s good news came as its rival, Merck, awaited word on authorization of its own antiviral pill for Covid, known as molnupiravir. In October, Merck and its partner Ridgeback Biotherapeutics announced that preliminary data showed the pill reduced the risk of hospitalization and death from Covid-19 by 50 percent, if taken within five days of the onset of symptoms.
But once the companies carried out a final analysis on all their data, molnupiravir’s effectiveness dropped to 30 percent. At an F.D.A. advisory committee meeting last month, a number of experts reacted coolly to this modest effectiveness, especially given some concerns about the safety of the pill.
The committee narrowly voted in favor of molnupiravir’s authorization. But now, two weeks later, the F.D.A. has yet to announce whether it will do so. In the meantime, France has turned down Merck’s application, citing its modest effectiveness and concerns about safety. Britain authorized molnupiravir last month.
“I don’t think the Merck pills have a long life in the United States if the Pfizer pill turns out to work as well as the data would suggest and there’s enough supply,” said Dr. Walid Gellad, who directs the Center for Pharmaceutical Policy and Prescribing at the University of Pittsburgh.
Pfizer stands to make a huge amount of money from Paxlovid. The investment bank SVB Leerink estimated that the drug would bring in $24 billion in global revenue in 2022 and $33 billion in 2023. That would give Paxlovid one of the highest single-year sales of any medical product in history.
To date, only one other product has brought in more: Pfizer’s Covid vaccine.
