Advanced technologies have been used to solve a long-standing mystery about why some people develop serious illness when they are infected with the malaria parasite, while others carry the infection asymptomatically.
An international team used mass cytometry – an in-depth way of characterising individual cells – and machine learning to discover ‘immune signatures’ associated with symptomatic or asymptomatic infections in people infected with the Plasmodium vivax parasite. This uncovered an unexpected role for immune T cells in protection against malaria, a finding that could help to improve the development of much-needed malaria vaccines.
The research, which was published in the journal JCI Insight was led by WEHI’s Dr Lisa Ioannidis and Associate Professor Diana Hansen, in collaboration with Professor Ric Price from the Menzies School of Health Research, Darwin, and Dr Rintis Noviyanti from the Eijkman Institute for Molecular Biology, Indonesia.
At a glance
- Advanced technologies have revealed ‘immune signatures’ that differentiate immune responses that drive symptomatic or asymptomatic Plasmodium vivax malaria infections.
- The international collaboration revealed a previously unrecognised role for immune CD4 T cells in preventing serious disease and controlling asymptomatic infection of low parasite burden.
- The findings could guide to the development of better vaccines against malaria, a disease that kills hundreds of thousands of people around the world each year.
Variable immune responses
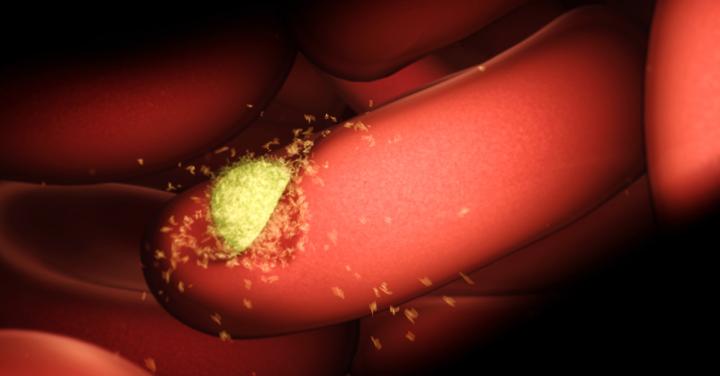
Malaria is a parasitic disease impacting hundreds of millions of people each year. After infection, people develop immunity to the Plasmodium parasite that causes malaria – but this immunity only reduces the disease severity rather than preventing infection altogether. Despite the immense global impact of malaria, there are not yet vaccines in clinical use to prevent this disease.
The immune response to malaria is a ‘double-edged sword’, Associate Professor Hansen said. “While an immune response to the parasite can prevent severe disease, in some people it is an excessive immune response – driving severe inflammation – that exacerbates malaria, causing the most severe, and potentially fatal, symptoms,” she said.
“Our research has investigated the longstanding question of how immune responses differ between people with symptomatic and asymptomatic malaria infections. We focussed on the Plasmodium vivax form of malaria, which is most common in the Asia-Pacific and Latin America. This species is a particular challenge to control as infected people can carry it for many months in the liver without symptoms.”
Using the University of Melbourne’s mass cytometry facility, the research team were able to undertake in-depth, multi-dimensional assessments of the immune cells in blood samples provided by people living in a vivax malaria-endemic region of Indonesia. Dr Ioannidis said the team compared many aspects of immunity in samples from people who were uninfected, asymptomatically infected, or symptomatically infected with P. vivax.
“In collaboration with a WEHI bioinformatics team led by Professor Gordon Smyth, we used machine learning to develop an ‘immune signature’ that distinguised between these three categories of samples. These signatures could be applied to new blood samples from people infected with malaria, to accurately predict the severity of their infection,” Dr Ioannidis said.
Enhancing malaria control
Dr Ioannidis said the immune signatures revealed the key components of the immune response that drive immunity to malaria. “Antibodies produced by B cells were one important component, especially in people with high parasite loads and symptomatic disease, but we also discovered that certain types of CD4 T cells were critical to keep infections in check, preventing symptoms,” she said.
“This is the first time CD4 T cells have been shown to be important for controlling asymptomatic P. vivax infections.”
Associate Professor Hansen said the discovery could lead to better approaches to controlling – or even eliminating – malaria. “Malaria vaccine development has focussed almost entirely on measuring antibody responses as a marker of vaccine success. Our research has revealed the important role of CD4 T cells in controlling malaria infections – and we think these cells need much more consideration when designing malaria vaccines. Because vivax malaria can persist in asymptomatic people, it is critical that vaccines activate CD4 T cells to control these low-grade infections,” Associate Professor Hansen said.
###
The research was supported by the Australian National Health and Medical Research Council, the Australian Academy of Science, the Wellcome Trust, the Indonesian Ministry of Research and Technology and the Victorian Government.
Disclaimer: AAAS and EurekAlert! are not responsible for the accuracy of news releases posted to EurekAlert! by contributing institutions or for the use of any information through the EurekAlert system.
