The oncoming flu season has claimed its first lives, among them a child in Florida who had not gotten a flu shot.
This year’s vaccine significantly reduces the odds of getting sick — and you should get one now if you haven’t already — but it’s far from perfect.
For one thing, its effectiveness fluctuates from year to year. At best, the vaccine may reduce the risk of illness by about 60 percent. Last year, during one of the worst flu epidemics in recent memory, that figure was just 40 percent.
And if a new strain of the flu were to strike, it might take months to develop an effective vaccine — plenty of time for the virus to sweep the globe, claiming hundreds of thousands, perhaps millions, of lives.
On Thursday, an international team of researchers offered a glimpse at something better than the seasonal flu shot. With a sophisticated combination of immunotherapy and gene therapy, they created an artificial antibody that protected mice against dozens of flu strains.
It’s an important step toward a type of flu shot that scientists have long sought: a shield against whatever flu strain people happen to pick up.
“There’s no one study that’s going to be the Holy Grail,” said Michael Osterholm, director of the Center for Infectious Disease Research and Policy at the University of Minnesota. “But there are going to be key studies upon which others can build. And this is one of them.”
Birds host a vast variety of flu strains, which are constantly mutating and mixing genes into new combinations. Sometimes these viruses manage to infect people; on occasion, they go on to evolve the molecular equipment necessary to travel from person to person.
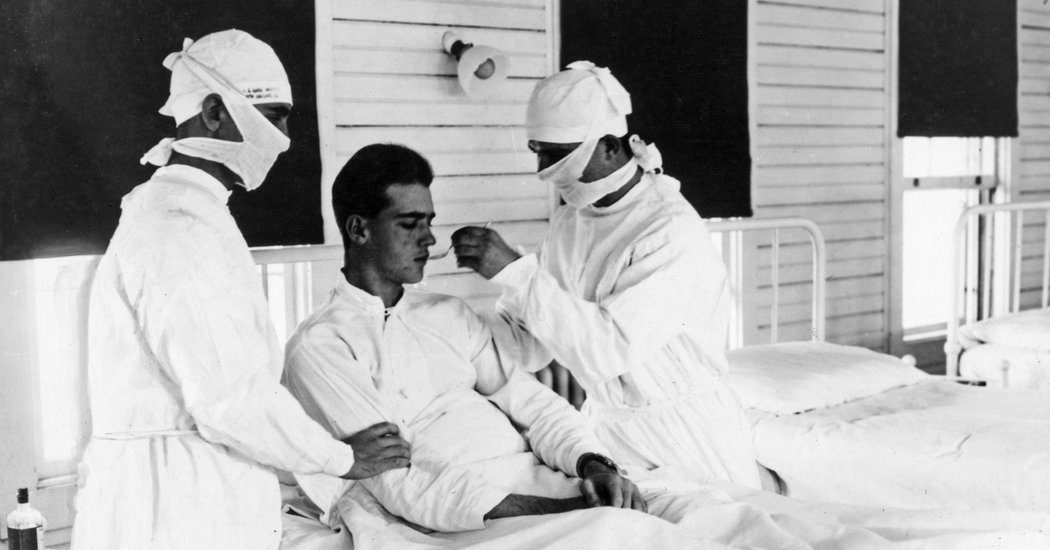
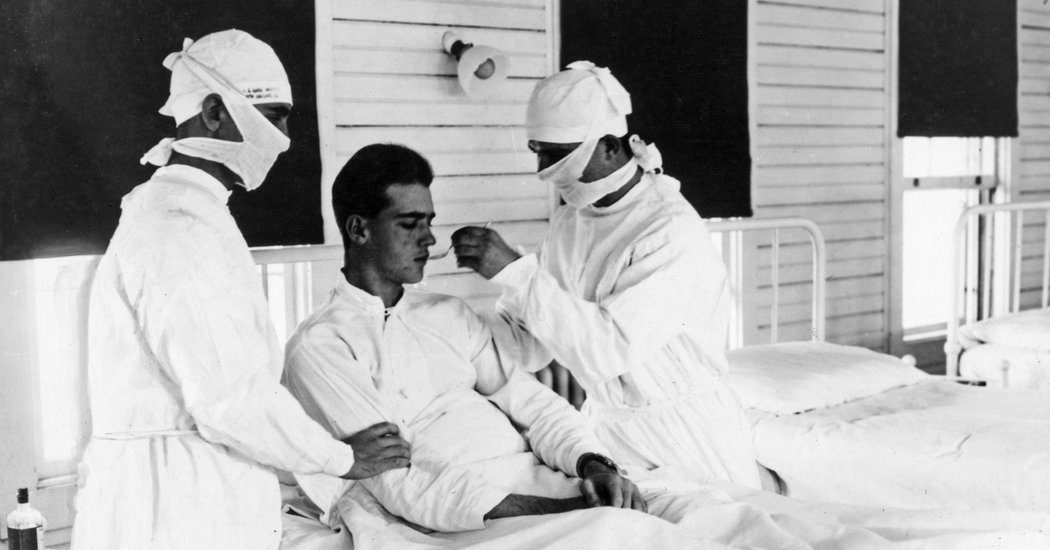
These catastrophic crossovers can cause pandemics. The worst one, in 1918, infected an estimated half-billion people and killed 50 million.
But at any given time, a number of less potent flu strains are circulating, killing as many as 646,000 people worldwide each year.
Vaccines significantly reduce the death toll by coaxing the immune system to make protective antibodies. These antibodies seek out a target on the virus: a knob on its shell (scientists often call it a spike) called hemagglutinin.
The antibodies attach to the tip of the knobs, making it difficult for flu viruses to enter cells. Unfortunately, each strain has a different sort of knob tip, and so an antibody effective against one flu strain often will not work against others.
Making matters worse, mutations can alter a strain’s hemagglutinin knob from one year to the next.
As a result, vaccine makers must guess which strain will dominate the coming flu season and plan accordingly.
Hope for a better vaccine emerged when scientists discovered that people sometimes produce rare antibodies that work against a range of flu strains. So-called broadly neutralizing antibodies don’t latch onto the tip of those viral knobs; instead, they target different parts — parts that are nearly identical from one viral strain to the next.
The authors of the new study wondered if they could string together these broadly neutralizing antibodies into a sort of mega-antibody. They isolated four of them, and then they created a gene that manufactured all four as a single mega-antibody.
The scientists then tested the creation against 60 flu strains spanning the genetic diversity of influenza. The mega-antibody grabbed tightly onto 59 strains, preventing them from multiplying in cells. (The only strain the mega-antibody didn’t work on is a type of bird flu that has never been known to infect people.)
“That’s something that made this quite a unique antibody,” said Joost A. Kolkman, an antibody engineer at Janssen, the pharmaceutical company, and a co-author of the new study, published in the journal Science. “We saw a coverage that has never been seen before.”
It would be impossible for a vaccine to coax our immune system into making this artificial creation. So the researchers tried an alternative strategy: sidestepping the immune system altogether.
The investigators loaded the gene into a harmless virus and sprayed it into the noses of mice. The viruses slipped into cells lining the nasal cavity, and they began producing mega-antibodies.
Then the real test: The scientists sprayed flu viruses into the nostrils of the mice. The team used some of the deadliest strains and delivered what should have been a lethal dose of each.
But the new antibodies grabbed hold of the viruses and prevented them from multiplying. The treated mice were entirely protected from lethal doses of the flu.
Kevin Hollevoet, a bioengineer at Leuven University in Belgium who was not involved in the new study, noted that this strategy has been used to produce antibodies against other infections, such as H.I.V.
“I’m not surprised that it also works for flu,” said Dr. Hollevoet. But earlier studies relied on antibodies naturally made by the immune system, he added. Coaxing mice to make a complicated, engineered antibody “is certainly an upgrade.”
But success in mice is no guarantee of success in people.
[Like the Science Times page on Facebook. | Sign up for the Science Times newsletter.]
For one thing, the antibodies that the researchers used to create their mega-antibody come from llamas, rather than people. The researchers gave the llamas flu vaccines and then gathered antibodies from their blood, including some that were effective against more than one strain.
Their choice of llamas was very practical. Llamas and related mammals have evolved to make small antibodies, making it easier to snap them together into a mega-antibody.
But it’s possible that the human immune system will look at antibodies from llamas as foreign. If so, they might attack, causing a potentially dangerous reaction.
Human trials will be needed to determine how safe the new antibodies are. Even if it pans out, scientists would have to figure out what dose is effective in people, as opposed to mice.
Still, given the toll of seasonal flu and the potential devastation of a new pandemic, Dr. Hollevoet hoped that the new experiment would spur more research.
“I hope it doesn’t take them ten years to push it forward,” he said.
Advancing flu vaccine research further will require a bigger commitment, Dr. Osterholm said. He noted that last year the United States government only spent $100 million on the field as a whole. “I would argue that’s not nearly enough,” he said.
Not only does war on flu need more funds, Dr. Osterholm added, but it needs more coordination between researchers, pharmaceutical companies and philanthropists.
“Who’s going to provide the air-traffic control leadership?” he asked.