Times Insider delivers behind-the-scenes insights into how news, features and opinion come together at The New York Times.
As a medical reporter, I frequently write about patients whose situations illustrate the points of my articles. Data and statistics often are the real story, but what we remember are the people and their poignant experiences.
And readers respond. I have heard from readers who want to help the patients, and from those who want me to tell their own stories. I have also heard from critics who have said the patients are just mouthpieces for drug companies.
But I have never had a response like the one I got to an article I wrote about powerful new cholesterol-lowering drugs. It came from the very top: the leaders of one of the two companies making the drugs.
In my story, I included two patients, Mackenzie Ames and Rodney Scheidel, who had very high levels of LDL cholesterol (the dangerous kind) and were at high risk for heart attacks — in fact, Mr. Scheidel had already had a heart attack. They needed the drugs, known as PCSK9 inhibitors. But their insurers had denied them coverage.
They, like many others, were caught in a battle between insurers, who want lower prices for these expensive drugs, and drug companies, who set the prices and negotiate deals with insurers. To put pressure on the two companies that make PCSK9 inhibitors, Amgen and Sanofi-Regeneron, insurers have made it very hard for patients to get the drugs.
My story was published on Oct. 2. That night, I got an email from Regeneron’s two founders and presidents: Dr. George D. Yancopoulos, who is also the company’s chief scientific officer, and Dr. Leonard S. Schleifer, who is also its chief executive officer.
They wrote: “If you can, please put Mackenzie and Rodney in touch with us, and we will try and help them get covered, or we can arrange to give them the drug for free.” They added: “While we can’t give everyone free drug, we can help Mackenzie and Rodney, especially as they had the courage to step forward and share their experiences.”
In a subsequent email, Dr. Yancopoulos provided his personal phone number and asked me to give it to the two patients, explaining that he can be slow answering emails.
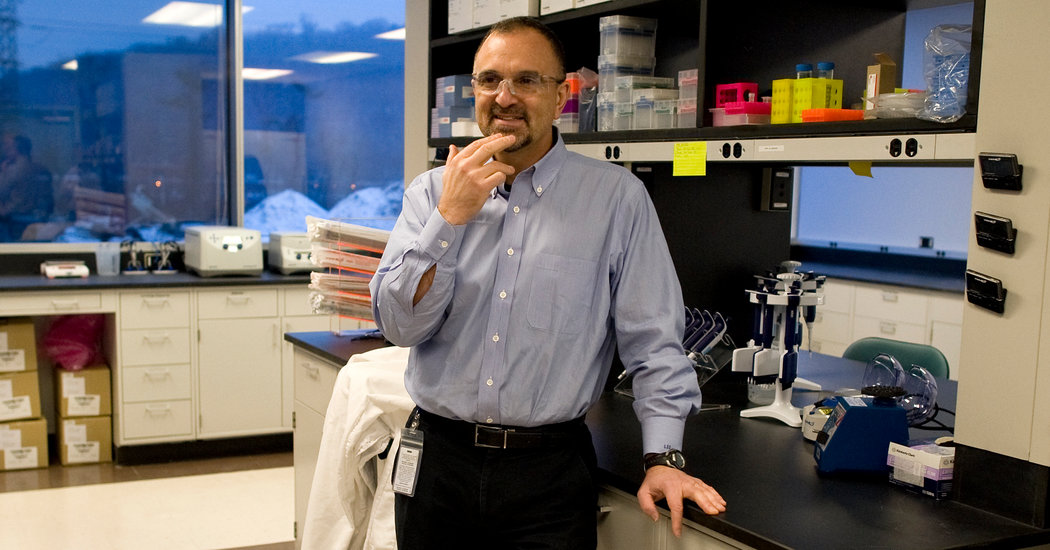
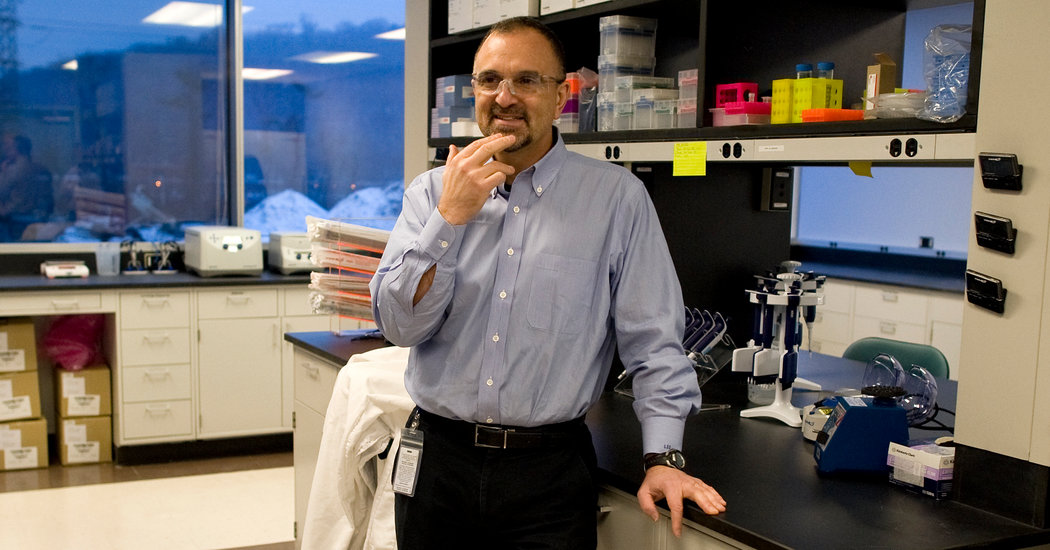
I called Dr. Yancopoulos the next day and, in an hourlong conversation, he passionately defended Regeneron and what it does. He also told me a remarkable tale about lack of access to PCSK9 inhibitors within Regeneron itself.
He and Dr. Schleifer both have M.D. and Ph.D. degrees — they are scientists who founded Regeneron in 1988, inspired, Dr. Yancopoulos said, by family members with debilitating diseases and their own experience treating patients with such diseases. Dr. Schleifer gave the company its motto: “Doing well by doing good.”
Twenty years later, Regeneron got its first drug approved. Five years after that, Regeneron finally made a profit.
During those lean years, Dr. Yancopoulos said, “Len and I were literally mocked. Analysts said, ‘This is what you get when you put scientists in charge of companies.’”
The company began working on its PCSK9 inhibitor, Praluent, in the early 2000s.
When it came time for human clinical trials, Regeneron partnered with Sanofi to conduct these very expensive tests. The drug worked beautifully, as did a similar drug made by Amgen: Repatha.
The total cost of developing Praluent and getting it approved was $2.6 billion, Dr. Yancopoulos said, adding that Sanofi-Regeneron made just $195 million last year in global sales.
The sales number was low, he said, in part because insurers balked at the price — the list price is more than $14,000 a year, although insurers negotiate substantial discounts — and in part because so many people were eligible that insurers were concerned, so they limited access. There have been estimates that as many as 10 million Americans could qualify to take Praluent or Repatha.
Dr. Yancopoulos believes so strongly in Praluent that he takes it himself, off-label. (He emphasizes that he is not suggesting others do that.) He has heart disease in his family, so even though his cholesterol level is not high enough for him to qualify — he declined to say what it is — he decided to pay Praluent’s full list price out of pocket to get his LDL as low as possible.
Yes, even though he is an inventor of Praluent and the chief scientific officer of Regeneron, he had to buy the drug at its full list price.
But the access issue really hit home, Dr. Yancopoulos said, when Regeneron’s own insurer denied Praluent to many of the company’s own employees who qualified for the drug.
So Regeneron put a new policy in place: The company would pay for any Regeneron drug for any company employee who had a doctor’s prescription and was unable to get the drug through Regeneron’s health insurance.
Since Dr. Yancopoulos has a doctor’s prescription for Praluent, he is a beneficiary of the policy.
And now, he says, he will be sure that Ms. Ames and Mr. Scheidel are too — unless their insurers relent and let them have the drug.
As a reporter, of course, I don’t get involved with special pleadings for patients, so I am staying out of this one. But as a human being, I sincerely hope these two patients get the drugs they need.
Keep up with Times Insider stories on Twitter, via the Reader Center: @ReaderCenter.
Gina Kolata writes about science and medicine. She has twice been a Pulitzer Prize finalist and is the author of six books, including “Mercies in Disguise: A Story of Hope, a Family’s Genetic Destiny, and The Science That Saved Them.” @ginakolata • Facebook