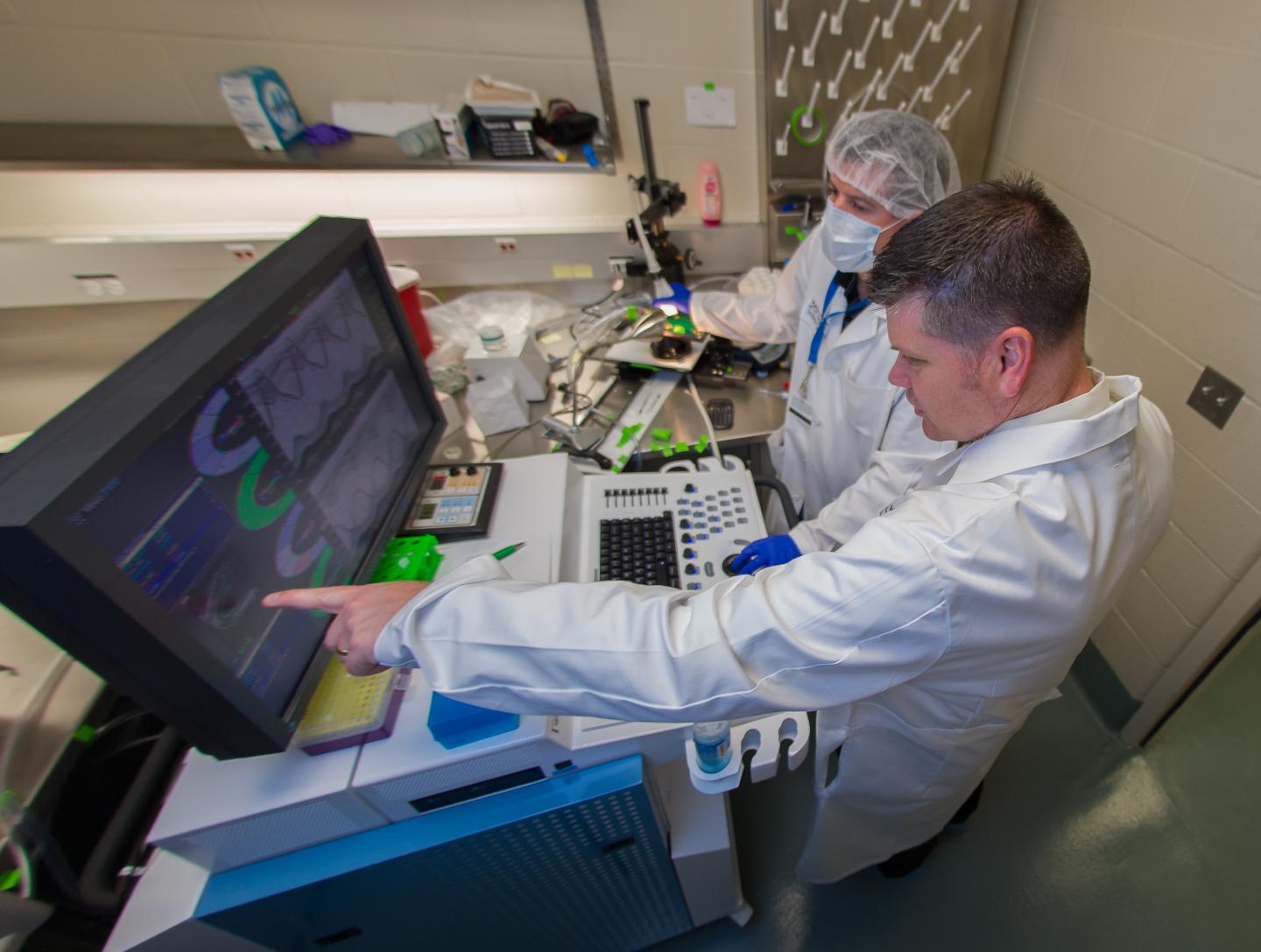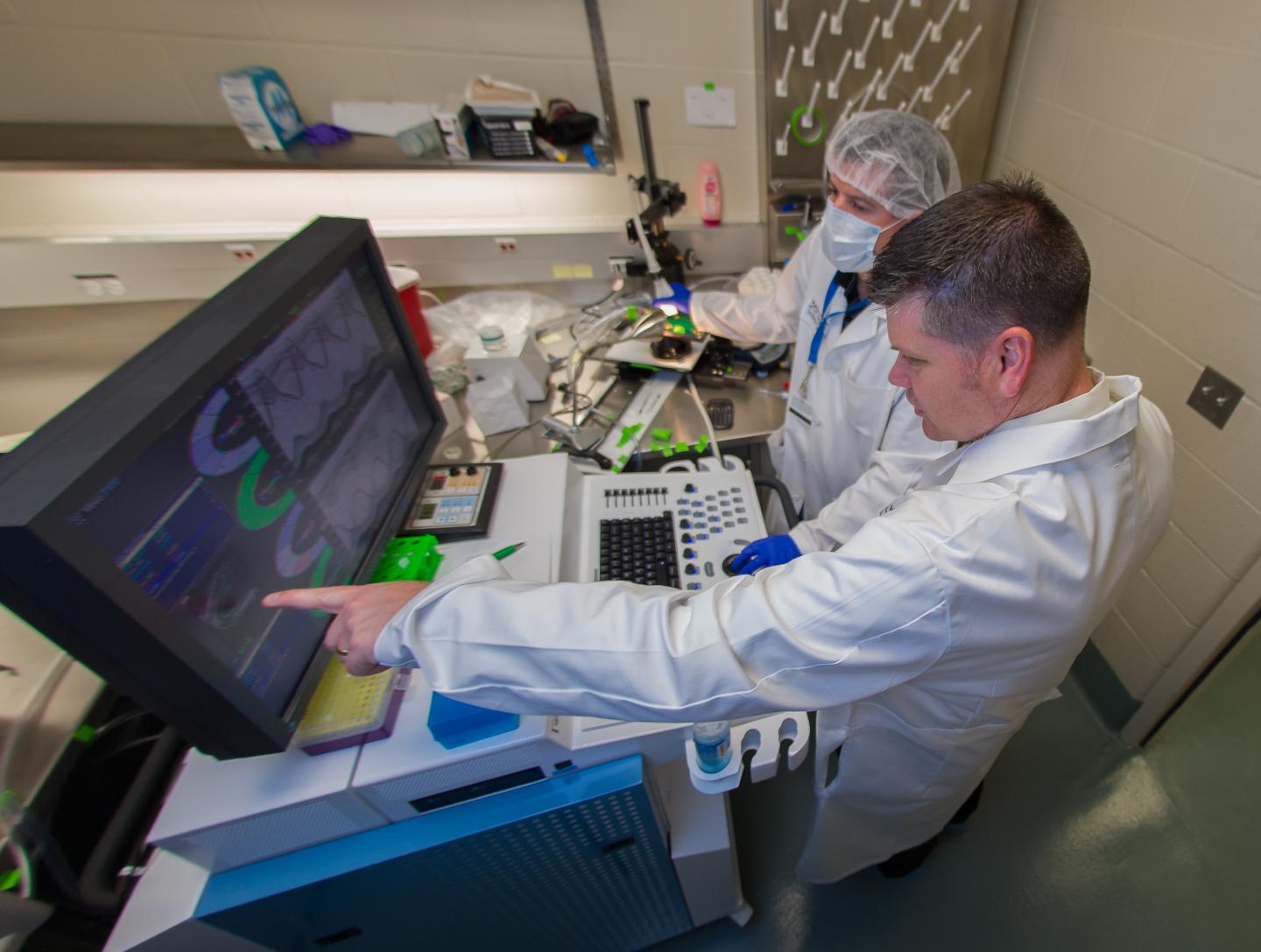
IMAGE: Gregory Aune, M.D., Ph.D., of UT Health San Antonio, (pointing) served on a team that found different chemotherapy drugs used to treat children with cancer appear to have different risks… view more
SAN ANTONIO — In long-term survivors of childhood cancer, cardiovascular disease is a leading cause of early death from non-cancer causes. In a new study, published Jan. 31 in JAMA Oncology, researchers compared four chemotherapy drugs with development of cardiomyopathy (abnormal heart muscle with impaired function) years after treatment.
“Exposure to anthracycline chemotherapies, such as doxorubicin, has long been associated with an increased risk of cardiovascular disease in long-term childhood cancer survivors,” said Gregory Aune, M.D., Ph.D., of UT Health San Antonio. “Previously, it was assumed that exposure to any member of the anthracycline class carried the same risk of late cardiovascular complications. By studying the outcomes of over 28,000 long-term survivors in the U.S. and Europe, this research indicates that exposure to different anthracyclines results in variable long-term cardiovascular risk. In the future, it will be important to take these differences into account when screening long-term survivors for cardiovascular complications and in the development of modern treatment regimens.”
The drug daunorubicin was associated with decreased cardiomyopathy risk when compared to doxorubicin, the study showed. Mitoxantrone, another chemotherapy, appeared to have greater long-term cardiomyopathy risk than was previously estimated.
“The past several decades have been focused on devising combinations of drugs that work best for curing patients,” said Gail Tomlinson, M.D., Ph.D., professor of pediatrics, division director of pediatric hematology-oncology, and holder of the Greehey Distinguished Chair in Genetics and Cancer at UT Health San Antonio. “This has been a highly successful process with a substantial increase in survival for most cancer types. Now with so many survivors alive many years from their original cancer, it is imperative to fine-tune protocols based on the goal of minimizing late effects.”
Dr. Aune, assistant professor of pediatric hematology-oncology at UT Health San Antonio and an investigator with the university’s Greehey Children’s Cancer Research Institute, assisted in the study design and review. Co-authors are from the Netherlands; the Fred Hutchinson Cancer Research Center in Seattle; St. Jude Children’s Research Hospital in Memphis, Tenn.; the Duke University School of Medicine; and the University of Washington, Seattle.
###
The University of Texas Health Science Center at San Antonio, now called UT Health San Antonio®, is one of the country’s leading health sciences universities. With missions of teaching, research, healing and community engagement, its schools of medicine, nursing, dentistry, health professions and graduate biomedical sciences have produced 36,500 alumni who are leading change, advancing their fields and renewing hope for patients and their families throughout South Texas and the world. To learn about the many ways “We make lives better®,” visit //www.
Stay connected with UT Health San Antonio on Facebook, Twitter, LinkedIn, Instagram and YouTube.
Disclaimer: AAAS and EurekAlert! are not responsible for the accuracy of news releases posted to EurekAlert! by contributing institutions or for the use of any information through the EurekAlert system.