A team of scientists announced Monday that they had partially restored the sight of a blind man by building light-catching proteins in one of his eyes. Their report, which appeared in the journal Nature Medicine, is the first published study to describe the successful use of this treatment.
“Seeing for the first time that it did work — even if only in one patient and in one eye — is exciting,” said Ehud Isacoff, a neuroscientist at the University of California, Berkeley, who was not involved in the study.
The procedure is a far cry from full vision. The volunteer, a 58-year-old man who lives in France, had to wear special goggles that gave him the ghostly perception of objects in a narrow field of view. But the authors of the report say that the trial — the result of 13 years of work — is a proof of concept for more effective treatments to come.
“It’s obviously not the end of the road, but it’s a major milestone,” said Dr. José-Alain Sahel, an ophthalmologist who splits his time between the University of Pittsburgh and the Sorbonne in Paris.
Dr. Sahel and other scientists have tried for decades to find a cure for inherited forms of blindness. These genetic disorders rob the eyes of essential proteins required for vision.
When light enters the eye, it is captured by so-called photoreceptor cells. The photoreceptors then send an electrical signal to their neighbors, called ganglion cells, which can identify important features like motion. They then send signals of their own to the optic nerve, which delivers the information to the brain.
In previous studies, researchers have been able to treat a genetic form of blindness called Leber congenital amaurosis, by fixing a faulty gene that would otherwise cause photoreceptors to gradually degenerate.
But other forms of blindness can’t be treated so simply, because their victims lose their photoreceptors completely. “Once the cells are dead, you cannot repair the gene defect,” Dr. Sahel said.
For these diseases, Dr. Sahel and other researchers have been experimenting with a more radical kind of repair. They are using gene therapy to turn ganglion cells into new photoreceptor cells, even though they don’t normally capture light.
The scientists are taking advantage of proteins derived from algae and other microbes that can make any nerve cell sensitive to light.
In the early 2000s, neuroscientists figured out how to install some of these proteins into the brain cells of mice and other lab animals by injecting viruses carrying their genes. The viruses infected certain types of brain cells, which then used the new gene to build light-sensitive channels.
Originally, researchers developed this technique, called optogenetics, as a way to probe the workings of the brain. By inserting a tiny light into the animal’s brain, they could switch a certain type of brain cell on or off with the flick of a switch. The method has enabled them to discover the circuitry underlying many kinds of behavior.
Dr. Sahel and other researchers wondered if they could use optogenetics to add light-sensitive proteins to cells in the retina. After all, they reasoned, retinal cells are nerves as well — an extension of the brain, in other words.
For Ed Boyden, a neuroscientist at M.I.T. who helped pioneer the field of optogenetics, the quest to use these proteins to cure blindness took him by surprise. “So far, I’ve thought of optogenetics as a tool for scientists primarily, since it’s being used by thousands of people to study the brain,” he said. “But if optogenetics proves itself in the clinic, that would be extremely exciting.”
Dr. Sahel and his colleagues recognized that the optogenetic proteins created by Dr. Boyden and others were not sensitive enough to produce an image from ordinary light entering the eye. But the scientists could not beam amplified light into the eye, because the glare would destroy the delicate tissue of the retina.
So the scientists chose an optogenetic protein that’s sensitive only to amber light, which is easier on the eye than other colors, and used viruses to deliver these amber proteins to the ganglion cells in the retina.
Next, the researchers invented a special device to transform visual information from the external world into amber light that could be recognized by the ganglion cells. They created goggles that scan their field of view thousands of times a second and register any pixels in which the light changes. The goggles then send a pulse of amber light from that pixel into the eye.
The researchers reasoned that this strategy might be able to create images in the brain. Our eyes naturally dart around in tiny movements many times a second. With each jump, many pixels would change light levels.
Still, it was an open question whether blind people could learn to use this information to recognize objects. “The brain has to learn a new language,” said Botond Roska, an ophthalmologist at the University of Basel and a co-author of the new study.
After testing their gene therapy and goggles on monkeys, Dr. Roska, Dr. Sahel and their colleagues were ready to try it out on people. Their plan was to inject gene-bearing viruses into one eye of each blind volunteer, then wait several months for the ganglion cells to grow optogenetic proteins. They would then train the volunteers to use the goggles.
Unfortunately, they only managed to train one volunteer before the coronavirus pandemic shut down the project. After years of preparation for the study, it was now stuck in limbo.
But then the one volunteer they had managed to train got in touch. For seven months, he had been wearing the goggles at home and on walks. One day he realized he could see the stripes of a crosswalk.
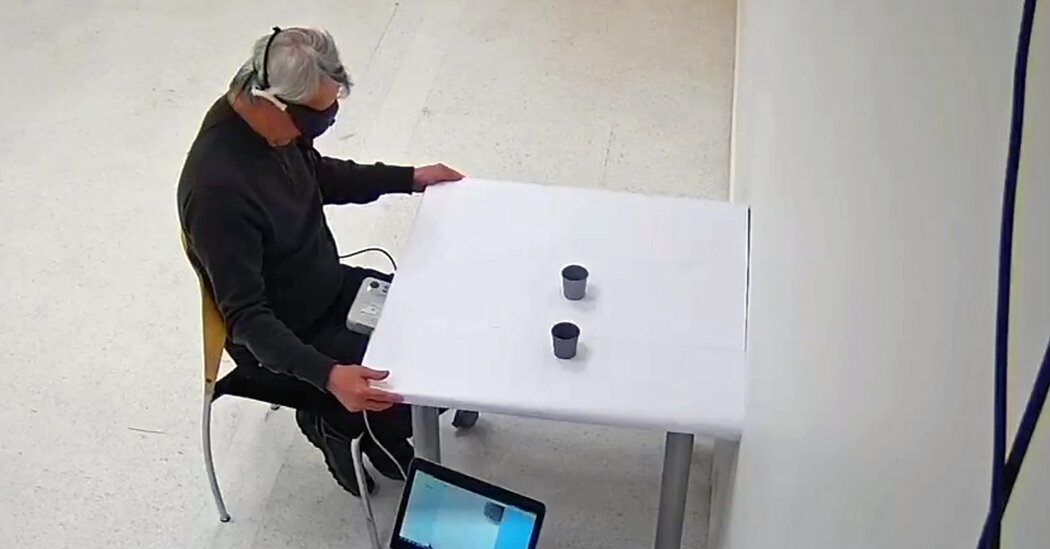
When the pandemic subsided in France over the summer, the scientists managed to bring him into their lab for more training and tests. They discovered that he could reach out and touch a notebook sitting on a table, but had less luck with a smaller box of staples. When the scientists set out either two or three tumblers in front of the volunteer, he managed to count them correctly 12 out of 19 times.
During some of the trials, the volunteer wore a cap with electrodes that could detect brain activity through his scalp. When the goggle sent signals to his retina, it activated parts of the brain involved in vision.
“It is a major achievement from a scientific point of view, and most importantly for blind people,” said Lucie Pellissier, a neuroscientist at the University of Tours in France who was not involved in the study.
Dr. Sahel and his colleagues founded a company called GenSight to move their technique through clinical trials with the hopes of getting it approved by regulators. They’re not alone. Dr. Isacoff and his colleagues have founded a similar company called Vedere Bio that was acquired last October by Novartis.
It will take many more positive results from clinical trials before optogenetics can become a standard treatment for some forms of blindness. For now, Dr. Sahel and his colleagues are bringing in the other volunteers for training, as well as testing higher doses of the virus and upgrading their goggles to thin spectacles that would be more comfortable while also delivering more information to the retina.
Dr. Isacoff and his colleagues have carried out experiments of their own that raise the possibility that other optogenetic proteins could make retinal cells sensitive enough to detect light without the help of goggles. “I think it’s going to perform quite well,” he said.
For all the time that Dr. Sahel has put into his own system, he hesitated to guess how far it could improve. “Until you have a patient tell you what they are seeing, you really can’t predict anything,” he said.
