Q. What is a fecal transplant, and why would I want one?
A. Fecal transplant is a medical procedure in which stool from a healthy donor is introduced into the intestine of a patient as a treatment for a disease. The idea is that the stool from the donor contains a healthful mix of gut bacteria that can seed the intestine of the patient, bringing healthful results.
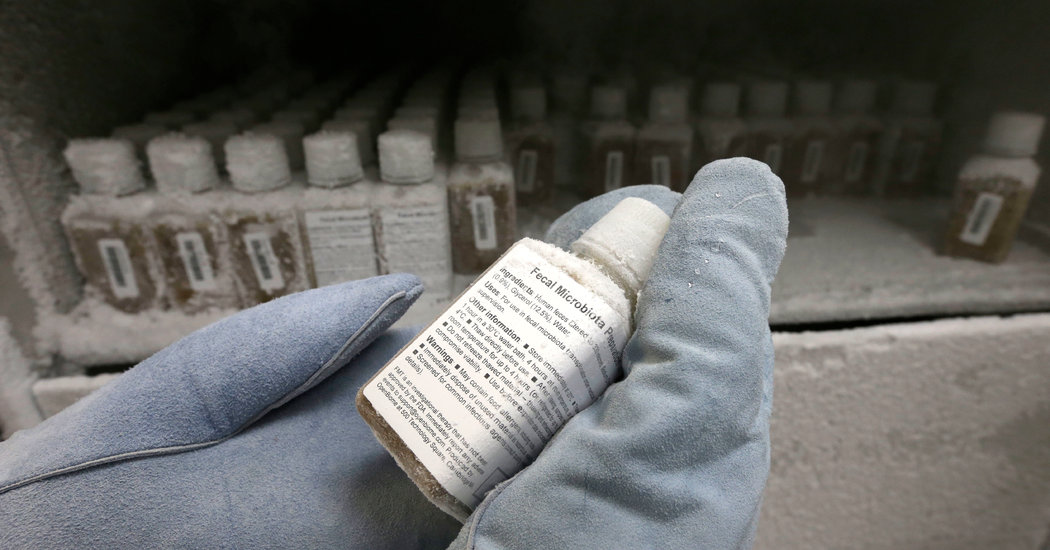
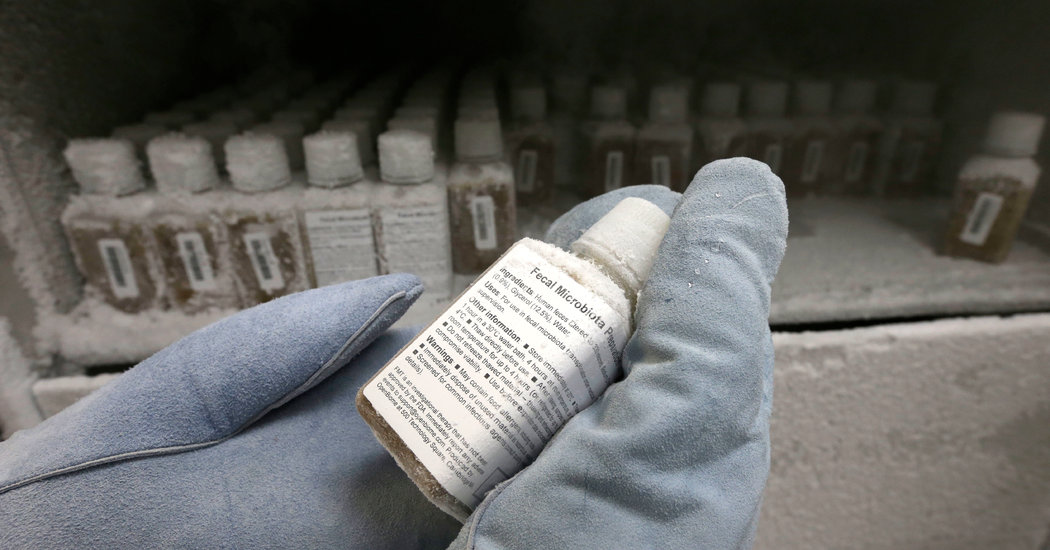
While the procedure may sound highly unappealing, it is not unsanitary. Stool is obtained from a donor or from a stool bank, where it has been screened for pathogens and processed for medical use.
Donor stool may be administered via a plastic tube inserted through the nose into the stomach or small intestine. Alternatively, donor stool may be introduced into the colon via an enema or colonoscopy, or by swallowing a capsule of stool.
Fecal transplant is used as a treatment for a serious infection of the colon with Clostridium difficile, a harmful bacterium that can take hold if antibiotics kill off enough of a person’s “good” gut bacteria. In 2011, C. diff caused some half a million infections, 29,000 deaths and $4.8 billion in health care costs in the United States alone.
A watershed moment in the use of fecal transplant, or what’s known in the medical literature as fecal microbiota transplant, occurred in 1958, when doctors tried the procedure as a last-ditch, heroic measure in four patients with life-threatening C. diff. Remarkably, all four patients survived. The results were described as “immediate and dramatic,” but because of a general revulsion to the thought of ingesting stool, fecal transplant still failed to win mainstream acceptance.
The tipping point occurred in 2013, with the publication of a landmark study showing fecal transplant to be superior to vancomycin, the current gold standard treatment for C. diff. Larger studies soon confirmed and extended these results.
Fecal transplant is now being studied as a treatment for obesity, recurrent urinary tract infections, ulcerative colitis, irritable bowel syndrome and a host of other conditions.
The preliminary data are encouraging, but enthusiasm must be tempered. The Food and Drug Administration regards fecal transplant as an “investigational new drug” and has not approved it for general use. Medical insurers typically cover fecal transplant only as a treatment for recurrent, intractable C. diff.
Reported side effects have been mild and include diarrhea, cramps, nausea, constipation and flatulence, though the trials performed to date have not been large enough to detect potentially more serious problems.
Experts offer this final piece of sage advice: “It is not recommended to perform stool transplantation at home without guidance from a physician.”
Do you have a health question? Ask Well