Heart disease remains the largest killer in Australia and around the world. A new study has shown that a protein therapy- recombinant human platelet-derived growth factor-AB (rhPDGF-AB) – could improve outcomes following heart attack.
After a heart attack, scar tissue forms and this negatively affects heart function. Now, researchers from The Westmead Institute for Medical Research (WIMR) and the University of Sydney found that, infusing rhPDGF into subjects that have had heart attacks improves the quality of the scar, leads to the formation of new blood vessels in the heart, and reduced rates of dangerous heart arrhythmia (irregularities of heart rhythm that can cause sudden death).
This study was in a pre-clinical large animal model.
The discovery publishes today in the leading journal Science Translational Medicine.
Corresponding author who led the research team, Associate Professor James Chong, said: “This is an entirely new approach with no current treatments able to change scar in this way.
“By improving cardiac function and scar formation following heart attack, treatment with rhPDGF-AB led to an overall increase in survival rate in our study.
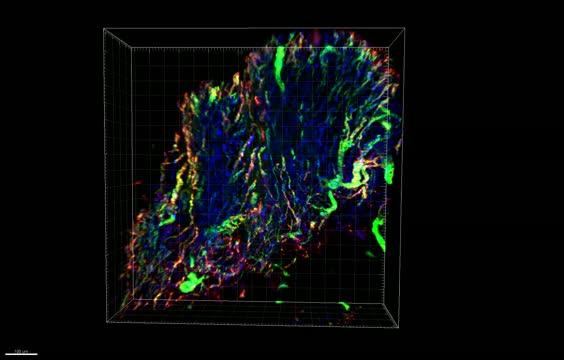
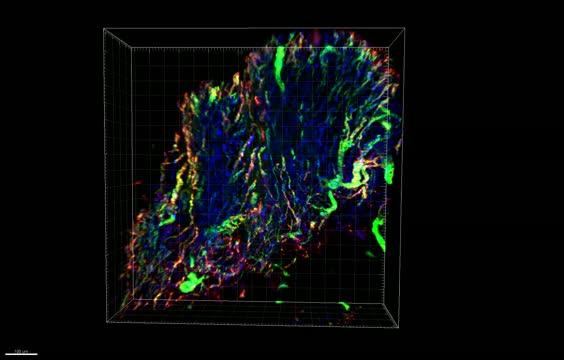
“While the treatment did not affect overall scar size, importantly we found that rhPDGF-AB led to increased scar collagen fibre alignment and strength. This improved heart function after the heart attack.
“Our collaborator Professor Richard Harvey,from the Victor Chang Cardiac Research Institute, had previously shown that the protein can improve heart function in mouse models following heart attack.
“This project has been developed over more than 10 years and we now have compelling data in two species for the effectiveness of this treatment.
Following heart attack, the heart muscle is damaged, causing thick scar tissue to form. This can limit the heart’s ability to function efficiently, and can increase the risk of heart failure, and sudden cardiac death.
Current treatments aim to restore blood and the oxygen supply to the heart as quickly as possible to reduce scarring. While this improves clinical outcomes, up to a quarter of patients experiencing their first heart attack will develop heart failure within one year.
Associate Professor Chong said: “While we have treatment protocols in place, it’s clear that there is an urgent, unmet need for additional treatments to improve patient outcomes particularly after large heart attacks.
“Heart disease is the leading cause of death in Australia. It is thought that more than 400,000 Australians have had a heart attack at some stage in their lives and that there is roughly one heart attack every 10 minutes. Through our research, we have the opportunity to change the negative impact of these statistics.
“Some further animal studies are required to clarify safety and dosing. Then we can start looking towards clinical trials in humans very soon. rhPDGF-AB is clearly a promising therapeutic option, and could potentially be used alongside existing treatments to improve heart attack patient outcomes and survival rates.
“We now hope to further investigate the treatment, including whether it could be used in other organ systems impacted by scar tissue, such as the kidneys.”
###
Associate Professor James Chong is Co-Director of WIMR’s Centre for Heart Research and Leader of WIMR’s Cardiac Regeneration Group; a Cardiologist at Westmead Hospital; Associate Professor at the University to Sydney; Principle Investigator and Westmead Applied Research Centre (WARC).
This research was conducted in collaboration with University of Sydney, The Victor Chang Cardiac Research Institute, Westmead Hospital, Kolling Institute of Medical Research and QIMR Berghofer. It was made possible by funding from NSW Office of Health and Medical Research, Heart Foundation, NSW Cardiovascular Research Network and Stem Cells Australia.
Disclaimer: AAAS and EurekAlert! are not responsible for the accuracy of news releases posted to EurekAlert! by contributing institutions or for the use of any information through the EurekAlert system.